Family Resources in Resources in Colorado
- Colorado Department of Human Services (cdhs.colorado.gov) Resources and contacts
- Mental Health Colorado (mentalhealthcolorado.org) Helplines, support groups, and services for advocates, caregivers and individuals in crisis
- SMI Adviser: Suicide and Serious Mental Illness (SMI) (cdhs.colorado.gov) Assessment and safety planning and crisis response guide
- Find Care in Colorado (ownpath.co) Find licensed providers by zip code
- Colorado Crisis Services (coloradocrisisservices.org) Helpline to connect with crisis clinicians by region
- NAMI Colorado (namicolorado.org) Support groups, training, information
- Disability Law Colorado (disabilitylawco.org) Protection and advocacy for individuals with disabilities
- Colorado Coalition for the Homeless (coloradocoalition.org) Nonprofit provides helpline and resources for housing, employment and/or health care listed by city and county
- CDOC Offender Search (doc.state.co.us/oss) Find offenders by name or DOC number
- (doc.state.co.us/oss) (doc.state.co.us/oss) Find offenders by name or DOC number
- Colorado Bar Association (cobar.org) Legal assistance
How many people in Colorado have SMI?
individuals with severe mental illness.
individuals with SMI who receive treatment in a given year.
of the adult population is estimated living with a SMI in the United States.
State psychiatric hospital beds in Colorado
2023 total beds: 482
- Civil beds: 192
- Forensic beds: 290
2023 beds per 100,000 people: 8.3
Click here for more information about state psychiatric hospital beds in Colorado.
A minimum of 50 beds per 100,000 people is considered necessary to provide minimally adequate treatment for individuals with severe mental illness. Colorado fails to meet this minimum standard.
For Additional Information
Data is a powerful tool to advocate for change. Curious about a specific data point in your state? Reach out to us at ORPA@treatmentadvocacycenter.org
Fast Facts on SMI in Colorado
Deinstitutionalization, outdated treatment laws, discriminatory Medicaid funding practices, and the prolonged failure by states to fund their mental health systems drive those in need of care into the criminal justice and corrections systems.
20%
5,812
482
12 to 1
2021 Colorado State Mental Health Agency's expenditures
Every state receives block grant funding from the federal government to provide mental health services to their community. Below is some information about how these dollars are spent and compares to other state spending.
$285,407,470
54%
$2,000
0.9%
Colorado's Treatment Laws
COLO. REV. STAT. § 27-65-106: (1) An emergency mental health hold may be invoked under one of the following conditions: (a)(I) When a certified peace officer has probable cause to believe a person has a mental health disorder and, as a result of the mental health disorder, is an imminent danger to the person’s self or others or is gravely disabled, the certified peace officer may take the person into protective custody and transport the person to a facility designated by the commissioner for an emergency mental health hold. If such a facility is not available, the certified peace officer may transport the person to an emergency medical services facility. The certified peace officer may request assistance from a behavioral health crisis response team for assistance in detaining and transporting the person or an emergency medical services provider in transporting the person; or (II) When an intervening professional reasonably believes that a person appears to have a mental health disorder and, as a result of the mental health disorder, appears to be an imminent danger to the person’s self or others or appears to be gravely disabled, the intervening professional may cause the person to be taken into protective custody and transported to a facility designated by the commissioner for an emergency mental health hold. If such a facility is not available, the certified peace officer may transport the person to an emergency medical services facility. The intervening professional may request assistance from a certified peace officer, a secure transportation provider, or a behavioral health crisis response team for assistance in detaining and transporting the person, or assistance from an emergency medical services provider in transporting the person. (b)(I) When a person petitions the court in the county in which the respondent resides or is physically present requesting an evaluation of the respondent’s condition and alleging that the respondent appears to have a mental health disorder and, as a result of the mental health disorder, appears to be a danger to the respondent’s self or others or appears to be gravely disabled. (II) Any person who files a malicious or false petition for an evaluation of a respondent pursuant to this section is subject to criminal prosecution. (2) When a person is taken into custody pursuant to subsection (1) of this section, the person must not be detained in a jail, lockup, or other place used for the confinement of persons charged with or convicted of penal offenses. Unless otherwise required by law, a certified peace officer may transport the person to an emergency medical services facility or facility designated by the commissioner even if a warrant has been issued for the person’s arrest if the certified peace officer believes it is in the best interest of the person. The person must not be held on an emergency mental health hold for longer than seventy-two hours after the hold is placed or ordered. Nothing in this section prohibits an emergency medical services facility from involuntarily holding the person in order to stabilize the person as required pursuant to the federal “Emergency Medical Treatment and Labor Act”, 42 U.S.C. sec. 1395dd, or if the treating professional determines that the individual’s physical or mental health disorder impairs the person’s ability to make an informed decision to refuse care and the provider determines that further care is indicated. (…) (6)(a) Each person detained for an emergency mental health hold pursuant to this section shall receive an evaluation as soon as possible after the person is presented to the facility and shall receive such treatment and care as the person’s condition requires for the full period that the person is held. The evaluation may include an assessment to determine if the person continues to meet the criteria for an emergency mental health hold and requires further mental health care in a facility designated by the commissioner. The evaluation must state whether the person should be released, referred for further care and treatment on a voluntary basis, or certified for short-term treatment pursuant to section 27-65-109. (b) Each evaluation must be completed using a standardized form approved by the commissioner and may be completed by a professional person; a licensed advanced practice registered nurse with training in psychiatric nursing; or a licensed physician assistant, a licensed clinical social worker, a licensed professional counselor, or a licensed marriage and family therapist who has two years of experience in behavioral health safety and risk assessment working in a health-care setting. (c) If the person conducting an evaluation pursuant to subsection (6)(a) of this section is not a professional person and the evaluating person recommends the detained person be certified for short-term treatment pursuant to section 27-65-109, the evaluating person shall notify the facility of the recommendation. A certification may only be initiated by a professional person. (7)(a) If a person is evaluated at an emergency medical services facility and the evaluating professional determines that the person continues to meet the criteria for an emergency mental health hold pursuant to subsection (1) of this section, the emergency medical services facility shall immediately notify the BHA if the facility cannot locate appropriate placement. Once notified, the BHA shall support the emergency medical services facility in locating an appropriate placement option on an inpatient or outpatient basis, whichever is clinically appropriate. (b) If an appropriate placement option cannot be located pursuant to subsection (7)(a) of this section and the person continues to meet the criteria for an emergency mental health hold pursuant to subsection (1) of this section and the person has been medically stabilized, the emergency medical services facility may place the person under a subsequent emergency mental health hold. If the facility places the person under a subsequent emergency mental health hold, the facility shall immediately notify the BHA, the person’s lay person, and the court, and the court shall immediately appoint an attorney to represent the person. The facility may notify the court where the person resides by mail. Once the court is notified, the emergency medical services facility is not required to take any further action to provide the person with an attorney unless specified in subsection (10) of this section. The emergency medical services facility shall notify the BHA after each emergency mental health hold is placed. The BHA is responsible for actively assisting the facility in locating appropriate placement for the person. If the person has been recently transferred from an emergency medical services facility to a facility designated by the commissioner and the designated facility is able to demonstrate that the facility is unable to complete the evaluation before the initial emergency mental health hold is set to expire, the designated facility may place the person under a subsequent emergency mental health hold and shall immediately notify the BHA and lay person.
COLO. REV. STAT. § 27-65-106(1). An emergency mental health hold may be invoked under one of the following conditions: (a)(I) When a certified peace officer has probable cause to believe a person has a mental health disorder and, as a result of the mental health disorder, is an imminent danger to the person’s self or others or is gravely disabled, the certified peace officer may take the person into protective custody and transport the person to a facility designated by the commissioner for an emergency mental health hold. If such a facility is not available, the certified peace officer may transport the person to an emergency medical services facility. The certified peace officer may request assistance from a behavioral health crisis response team for assistance in detaining and transporting the person or an emergency medical services provider in transporting the person (…) COLO. REV. STAT. § 27-65-102(10). "Danger to the person’s self or others" means: (a) A person poses a substantial risk of physical harm to the person’s self as manifested by evidence of recent threats of or attempts at suicide or serious bodily harm to the person’s self; or (b) A person poses a substantial risk of physical harm to another person or persons, as manifested by evidence of recent homicidal or other violent behavior by the person in question, or by evidence that others are placed in reasonable fear of violent behavior and serious physical harm to them, as evidenced by a recent overt act, attempt, or threat to do serious physical harm by the person in question. COLO. REV. STAT. § 27-65-102(17). “Gravely disabled” means a condition in which a person, as a result of a mental health disorder, is incapable of making informed decisions about or providing for the person’s essential needs without significant supervision and assistance from other people. As a result of being incapable of making these informed decisions, a person who is gravely disabled is at risk of substantial bodily harm, dangerous worsening of any concomitant serious physical illness, significant psychiatric deterioration, or mismanagement of the person’s essential needs that could result in substantial bodily harm. A person of any age may be “gravely disabled”, but the term does not include a person whose decision-making capabilities are limited solely by the person’s developmental disability.

COLO. REV. STAT. § 27-65-111. [Editor’s note: This section is effective July 1, 2024.] 1. Any respondent certified pursuant to section 27-65-109 or 27-65-110 may be provided treatment on an outpatient basis. The outpatient treatment provider shall develop a treatment plan for the respondent receiving treatment on an outpatient basis with the goal of the respondent finding and sustaining recovery. The treatment plan must include measures to keep the respondent or others safe, as informed by the respondent’s need for certification. The treatment plan may include, but is not limited to: a. Intensive case management; b. Assertive community treatment; c. Peer recovery services; d. Individual or group therapy; e. Day or partial-day programming activities; f. Intensive outpatient programs; g. Educational and vocational training or activities; and h. Housing and transportation assistance. 2. The respondent, the respondent’s legal guardian, the respondent’s patient representative or the respondent’s lay person, or any party at any court hearing may contest a respondent’s treatment regimen, including court-ordered medications, at any court hearing related to the respondent’s certification for treatment. 3. The facility responsible for providing services to a respondent on a certification on an outpatient basis shall proactively reach out to the respondent to engage the respondent in treatment. If the respondent refuses treatment or court-ordered medication and is decompensating psychiatrically, the court may order a certified peace officer or secure transportation provider to transport the respondent to an appropriate, least restrictive designated facility in collaboration with the BHA and the provider holding the certification. The respondent does not need to be imminently dangerous to the respondent’s self or others for the provider to request, and the court to order, transportation to a facility for the respondent to receive treatment and court-ordered medications. The facility responsible for providing services to a respondent on a certification on an outpatient basis shall provide the court information on the facility’s proactive outreach to the respondent and the professional person’s and psychiatric advanced practice registered nurse’s basis for medical opinion. 4. If a respondent is placed in a more restrictive setting, the respondent has the right to judicial review within ten days after filing a written request. 5. a. In addition to any other limitation on liability, a person providing care to a respondent placed on short-term or long-term certification on an outpatient basis is only liable for harm subsequently caused by or to a respondent who: 1. Has been terminated from certification despite meeting statutory criteria for certification pursuant to section 27-65-109 or 27-65-110; or 2. Provided services to the respondent not within the scope of the person’s professional license, or was reckless or grossly negligent in providing services. b. A provider is not liable if a respondent’s certification is terminated, despite meeting criteria for certification, if the provider is unable to locate the respondent despite proactive and reasonable outreach. 6. A respondent subject to a short-term or long-term certification on an outpatient basis has the following rights, in addition to those enumerated in section 27-65-119: 7. a. To request a change to voluntary status. A change to voluntary status may be denied by the supervising professional person or advanced practice registered nurse with training in psychiatric nursing responsible for the respondent’s treatment if the professional person or advanced practice registered nurse with training in psychiatric nursing determines reasonable grounds exist to believe that the respondent will not remain in a voluntary treatment program. b. To be treated fairly, with respect and recognition of the respondent’s dignity and individuality, by all employees of the treatment facility with whom the respondent comes in contact; c. To appropriate treatment, which must be administered skillfully, safely, and humanely. A respondent shall receive treatment suited to the respondent’s needs that must be determined in collaboration with the respondent. d. To not be discriminated against on the basis of age, race, ethnicity, religion, culture, spoken language, physical or mental disability, socioeconomic status, sex, sexual orientation, gender identity, or gender expression; e. To retain and consult with an attorney at any time; f. Within forty-eight hours after the respondent’s request, to see and receive the services of a patient representative, including a peer specialist, who has no direct or indirect clinical, administrative, or financial responsibility for the respondent; g. To have the respondent’s behavioral health orders for scope of treatment or psychiatric advance directive reviewed and considered by the court as the preferred treatment option for involuntary administration of medications unless, by clear and convincing evidence, the respondent’s directive does not qualify as effective participation in behavioral health decision-making; h. To have the respondent’s information and records disclosed to adult family members and a lay person pursuant to section 27-65-123; i. To have access to a representative within the facility who provides assistance to file a grievance; and j. To have the right to file a motion with the court at any time to contest the certification.
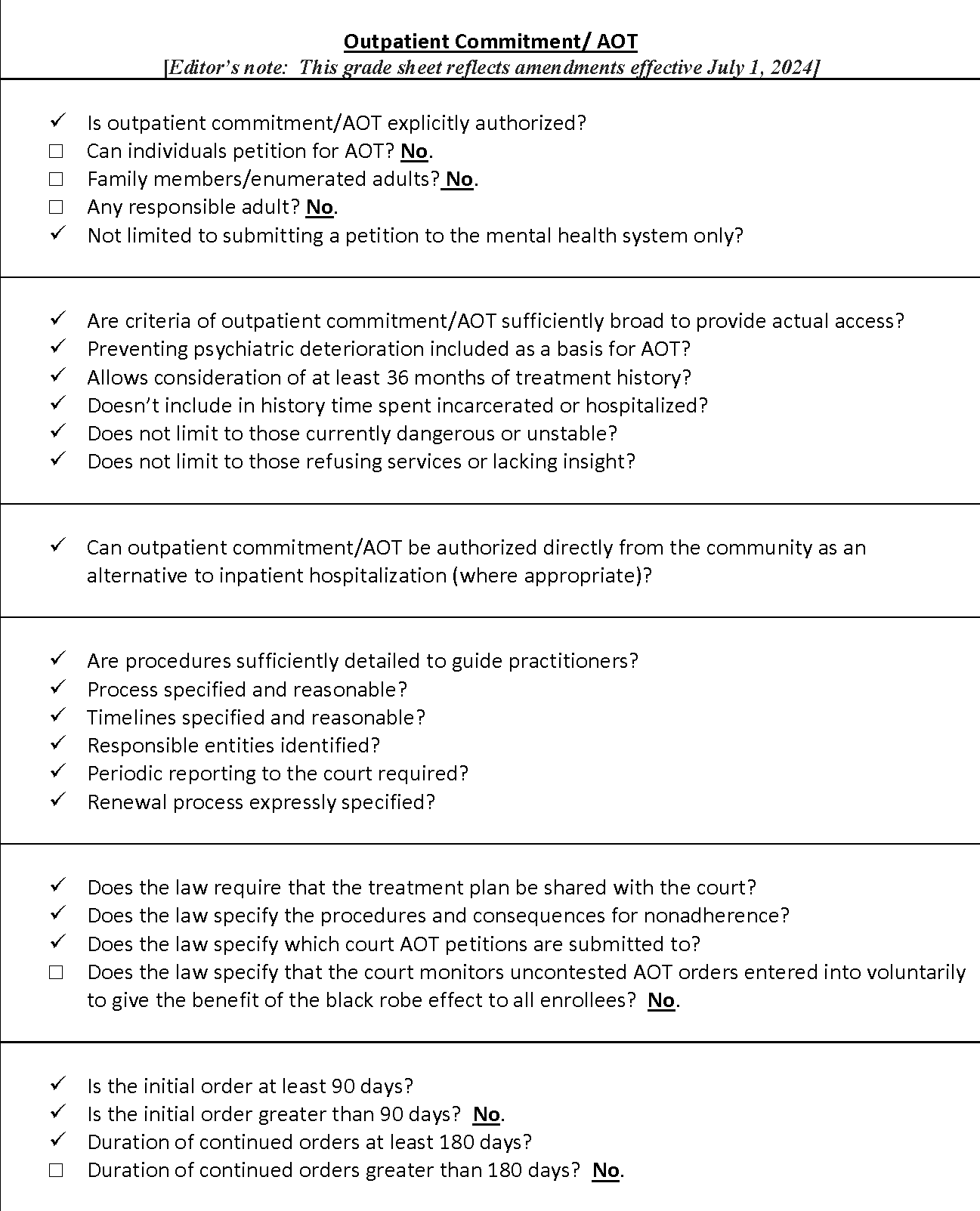
Recommended updates to treatment laws
- 1
Amend Colo. Rev. Stat. §§ 27-65-107 and 27-65-108 to authorize citizen right of petition for at least enumerated citizens, preferably any responsible adult, for inpatient commitment
- 2
Amend Colo. Rev. Stat. § 27-65-107 to authorize citizen right of petition for at least enumerated citizens, preferably any responsible adult, for outpatient commitment
- 3
Amend Colo. Rev. Stat. §§ 27-65-108 and 27-65-109 to extend duration of continued outpatient order beyond 180 days
- 4
Adopt express procedures for the court to monitor uncontested AOT orders entered into voluntarily to give the benefit of the black robe effect to all enrollees
