Family Resources in Resources in Oregon
- Oregon Health Authority Behavioral Health Services (oregon.gov/oha) Resources and contacts
- Mental Health Facilities in Oregon (mentalheatlhclinics.org) Inpatient and residential treatment options
- Early Assessment and Support Alliance (easacommunity.org) First episode psychosis programs with phone numbers by county for making a referral
- Office of Recovery and Resilience (oregon.gov/oha) Peer support services and help with understanding patient rights and how to file a complaint
- Psychiatric Security Review Board (PSRB) (Oregon.gov) Reintegration program for people found guilty except for insanity (GEI)
- Aid and Assist (Oregon.gov) Restoration services for people charged with a crime and found unable to act in their own defense
- NAMI Oregon (namior.org) Support groups, training, information
- Disability Rights Oregon (droregon.org) Protection and advocacy for individuals with disabilities
- Oregon Homeless Services Programs (oregon.gov) Program options and contacts
- Oregon Offender Search (docpub.state.or.us) Search for someone in prison by name and SID number
- Oregon State Bar (osbar.org) Legal assistance
How many people in Oregon have SMI?
individuals with severe mental illness.
individuals with SMI who receive treatment in a given year.
of the adult population is estimated living with a SMI in the United States.
State psychiatric hospital beds in Oregon
2023 total beds: 704
- Civil beds: 50
- Forensic beds: 654
2023 beds per 100,000 people: 16.6
Click here for more information about state psychiatric hospital beds in Oregon.
A minimum of 50 beds per 100,000 people is considered necessary to provide minimally adequate treatment for individuals with severe mental illness. Oregon fails to meet this minimum standard.
For Additional Information
Data is a powerful tool to advocate for change. Curious about a specific data point in your state? Reach out to us at ORPA@treatmentadvocacycenter.org
Fast Facts on SMI in Oregon
Deinstitutionalization, outdated treatment laws, discriminatory Medicaid funding practices, and the prolonged failure by states to fund their mental health systems drive those in need of care into the criminal justice and corrections systems.
18%
3,694
704
5 to 1
2021 Oregon State Mental Health Agency's expenditures
Every state receives block grant funding from the federal government to provide mental health services to their community. Below is some information about how these dollars are spent and compares to other state spending.
$1,503,065,393
19%
$9,460
2.3%
Oregon's Treatment Laws
OR. REV. STAT. § 426.228(1). A peace officer may take into custody a person who the officer has probable cause to believe [meets the criteria for emergency evaluation]. OR. REV. STAT. § 426.233(1)(b). [If a person is found to meet criteria for emergency evaluation, t]he community mental health program director or designee … may: (A) Notify a peace officer to take the person into custody and direct the officer to remove the person to a hospital or nonhospital facility approved by the Oregon Health Authority; (B) Authorize involuntary admission of, or, if already admitted, cause to be involuntarily retained in a nonhospital facility approved by the authority, a person approved for care or treatment at a nonhospital facility by a physician[;] (C) Notify an [authorized individual] to take the person into custody and direct the authorized individual to remove the person in custody to a hospital or nonhospital facility approved by the authority; (D) Direct an [authorized individual] to transport a person in custody from a hospital or a nonhospital facility approved by the authority to another hospital or nonhospital facility approved by the authority[;] or (E) Direct an [authorized individual] to transport a person in custody from a facility approved by the authority to another facility approved by the authority[.] OR. REV. STAT. § 426.232(1). If a licensed independent practitioner … believes a person who is at a hospital or nonhospital facility, is dangerous to self or to any other person and is in need of emergency care or treatment for mental illness, and the licensed independent practitioner is not related to the person by blood or marriage, the licensed independent practitioner may do one of the following: (a) Detain the person and cause the person to be admitted or, if the person is already admitted, cause the person to be retained in a hospital where the licensed independent practitioner has admitting privileges or is on staff. (b) Approve the person for emergency care or treatment at a nonhospital facility approved by the authority. OR. REV. STAT. § 426.228(1). A peace officer may take into custody a person who the officer has probable cause to believe is dangerous to self or to any other person and is in need of immediate care, custody or treatment for mental illness. OR. REV. STAT. § 426.233(1)(a). A community mental health program director … or a designee of the director may [seek emergency evaluation] when the community mental health program director or designee has probable cause to believe a person: (A) Is dangerous to self or to any other person and is in need of immediate care, custody or treatment for mental illness; or (B) (i) Is a person with mental illness placed on conditional release …, outpatient commitment … or trial visit[;] and (ii) Is dangerous to self or to any other person or is unable to provide for basic personal needs and is not receiving the care that is necessary for health and safety and is in need of immediate care, custody or treatment for mental illness.
OR. REV. STAT. § 426.070(1). Any of the following may initiate commitment procedures: (a) Two persons; (b) The county health officer; or (c) Any magistrate or judge of a court of a federally recognized Indian tribe located in this state. OR. REV. STAT. § 426.005(1)(f). "Person with mental illness" means a person who, because of a mental disorder, is one or more of the following: (A) Dangerous to self or others. (B) Unable to provide for basic personal needs that are necessary to avoid serious physical harm in the near future, and is not receiving such care as is necessary to avoid such harm. (C) A person: (i) With a chronic mental illness[;] (ii) Who, within the previous three years, has twice been placed in a hospital or approved inpatient facility by the [Oregon Health Authority] or the Department of Human Services[;] (iii) Who is exhibiting symptoms or behavior substantially similar to those that preceded and led to one or more of the hospitalizations or inpatient placements referred to in sub- subparagraph (ii) of this subparagraph; and (iv) Who, unless treated, will continue, to a reasonable medical probability, to physically or mentally deteriorate so that the person will become a person described under either or both subparagraph (A) or (B) of this paragraph or both.
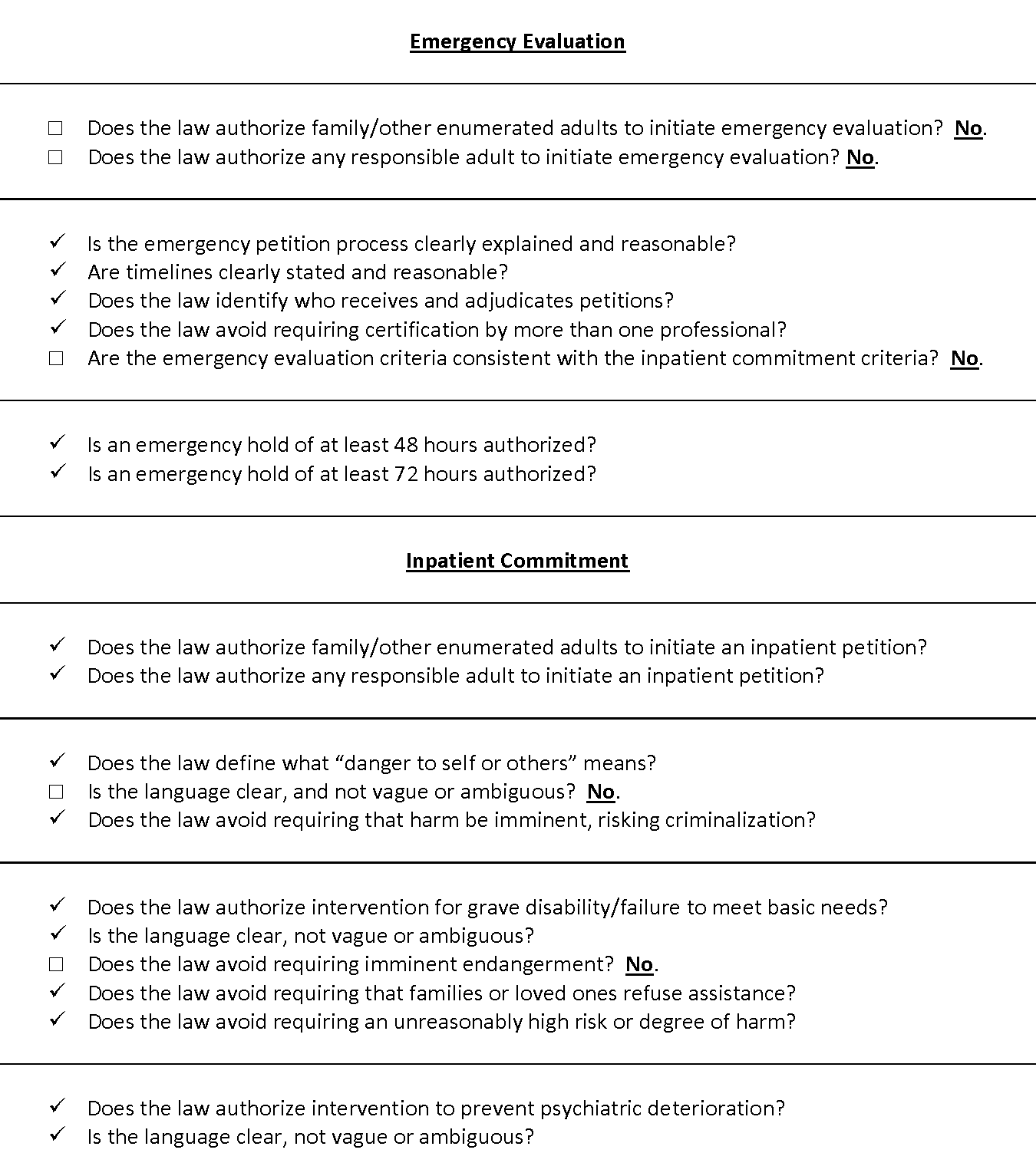
OR. REV. STAT. § 426.133(2). A court may issue an order requiring a person to participate in assisted outpatient treatment if the court finds that the person: (a) (A) Is 18 years of age or older; (B) Has a mental disorder; (C) Will not obtain treatment in the community voluntarily; and (D) Is unable to make an informed decision to seek or to comply with voluntary treatment; and (b) As a result of being a person described in paragraph (a) of this subsection: (A) Is incapable of surviving safely in the community without treatment; and (B) Requires treatment to prevent a deterioration in the person’s condition that will predictably result in the person becoming a person with mental illness. OR. REV. STAT. § 426.133(3). In determining whether to issue the order under subsection (2) of this section, the court shall consider, but is not limited to considering, the following factors: (a) The person’s ability to access finances in order to get food or medicine. (b) The person’s ability to obtain treatment for the person’s medical condition. (c) The person’s ability to access necessary resources in the community without assistance. (d) The degree to which there are risks to the person’s safety. (e) The likelihood that the person will decompensate without immediate care or treatment. (f) The person’s previous attempts to inflict physical injury on self or others. (g) The person’s history of mental health treatment in the community. (h) The person’s patterns of decompensation in the past. (i) The person’s risk of being victimized or harmed by others. (j) The person’s access to the means to inflict harm on self or others.

Recommended updates to treatment laws
- 1
Amend Or. Rev. Stat. §§ 426.228(1) and 426.233(1)(a) to authorize citizen right of petition for at least enumerated citizens, preferably any responsible adult, for emergency evaluation
- 2
Amend Or. Rev. Stat. §§ 426.228(1) and 426.233(1)(a) to remove inconsistency between emergency and inpatient criteria by expressly adding other bases for inpatient commitment to emergency standard
- 3
Amend Or. Rev. Stat. § 426.005(1)(f)(A) to provide adequate definition of danger to self or others
- 4
Amend Or. Rev. Stat. § 426.005(1)(f)(B) to remove imminence requirement to meet criteria for grave disability
- 5
Adopt express procedures for the court to monitor uncontested AOT orders entered into voluntarily to give the benefit of the black robe effect to all enrollees